Complications of Total Parenteral Nutrition (TPN)
I. Catheter-Related Complications:
-The
hyperosmolarity of the dextrose and amino acid solutions requires infusion
through large veins or central venous lines.
1-Misdirected
Catheter: e.g., with subclavian vein cannulations – (mostly on the right) 10%
resulted in misplacement of the catheter in the internal jugular vein.
2-Infection
3-Hematoma
4-Thrombosis
II. Carbohydrate Complications:
1-Hyperglycemia:
-Hyperglycemia
is common during TPN; blood glucose levels >300 mg/dl were recorded in 20% of
postoperative patients receiving TPN.
-A standard
TPN regimen with 1,800 non-protein calories has ≈350 g of glucose, compared to
230 g in a standard tube feeding regimen.
-Tight
glycemic control is not recommended in critically ill patients because of the
risk of hypoglycemia, which has more serious consequences than hyperglycemia.
-The current
recommendation for hospitalized patients is a target range of 140–180 mg% for
blood glucose.
2-Insulin:
-If insulin
therapy is required, regular insulin is preferred for critically ill patients,
to prevent wide swings in glucose levels, by adding insulin to the TPN
solutions.
-One
shortcoming of IV insulin infusions is the propensity for insulin to adsorb to
the plastic tubing in IV infusion sets. This affects the bioavailability of
insulin but can be reduced by priming the IV infusion set with an insulin
solution (e.g., 20 mL of saline containing 1 unit/mL of regular insulin). But
the priming procedure must be repeated each time the IV infusion set is
changed.
-SC insulin
can be used for stable patients. Regimens will vary in each patient, with a combination of intermediate or long-acting insulin with rapid-acting insulin,
when needed.
3-Hypophosphatemia:
-The movement
of glucose into cells is associated with a similar movement of phosphate into
cells, and this provides phosphate for co-factors (e.g., thiamine
pyrophosphate) that participate in glucose metabolism. This intracellular shift
of phosphate can result in hypophosphatemia.
4-Hypokalemia:
-Glucose
movement into cells is also accompanied by an intracellular shift of potassium
(which is the basis for the use of glucose and insulin to treat severe
hyperkalemia). This effect is usually transient, but continued glucose loading
during TPN can lead to persistent hypokalemia.
5-Hypercapnia:
-Excess
carbohydrate intake promotes CO2 retention in patients with
respiratory insufficiency. This was originally attributed to the high
respiratory quotient (VCO2/VO2) associated with
carbohydrate metabolism. However, CO2 retention is a consequence of
overfeeding, and not overfeeding with carbohydrates.
III. Lipid Complications:
-Overfeeding
with lipids may contribute to hepatic steatosis.
-Triggering
inflammatory response: The lipid emulsions used in TPN regimens are rich in
oxidizable lipids, and the oxidation of infused lipids will trigger an
inflammatory response. (Oleic acid, one of the lipids in TPN, is a standard
method for producing ARDS in animals), and this might explain why lipid
infusions are associated with impaired oxygenation.
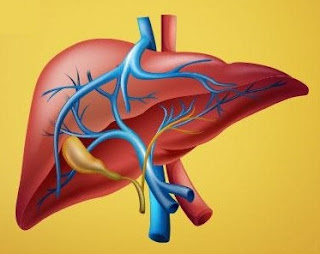
IV. Hepatobiliary Complications:
1-Hepatic Steatosis:
-Fat
accumulation in the liver (hepatic steatosis) is common in patients receiving long-term
TPN and is believed to be the result of chronic overfeeding with carbohydrates
and lipids. Although this condition is associated with elevated liver enzymes,
it may not be a pathological entity.
2-Cholestasis:
-The absence
of lipids in the proximal small bowel prevents cholecystokinin-mediated
contraction of the gallbladder. This results in bile stasis and the
accumulation of sludge in the gallbladder and can lead to acalculous
cholecystitis.
V. Bowel Sepsis:
-The absence
of nutritional bulk in the GI tract leads to atrophic changes in the bowel
mucosa and impairs bowel-associated immunity, and these changes can lead to
the systemic spread of enteric pathogens.