Airway Blocks
1-Superior laryngeal n. block:
Block of the superior laryngeal nerve can provide anesthesia of the larynx from the epiglottis to the level of the vocal cords. This block may be appropriate for any patient requiring TI before anesthetic induction.
Anatomy (Fig. 1):
The superior laryngeal n. is a branch of the vagus n. After it leaves the main vagal trunk, it courses through the neck and passes medially, caudal to the greater cornu of the hyoid bone, at this point, it divides into an internal and external branch. The internal branch is the nerve of interest in the superior laryngeal n. block, and it is blocked where it enters the thyrohyoid membrane inferior to the caudal aspect of the hyoid bone.
Technique (Fig. 1):
The patient is placed supine, with the neck extended. The anesthesiologist should displace the hyoid bone toward the side to be blocked by grasping it between the index finger and the thumb. A 25-gauge, short needle is then inserted to make contact with the greater cornu of the hyoid bone. The needle is walked off the caudal edge of the hyoid and advanced 2 to 3 mm so that the needle tip rests between the thyrohyoid membrane laterally and the laryngeal mucosa medially. 2-3 ml of lidocaine 0.5% is then injected; an additional 1 ml is injected while the needle is withdrawn.
 |
| Fig. 1: Superior Laryngeal n. Block |
2-Glossopharyngeal n. block:
Glossopharyngeal n. block is useful for anesthesia of the mucosa of the pharynx and soft palate and for eliminating the gag reflex that results when pressure is applied to the posterior third of the tongue, even after adequate topical mucosal anesthesia has been obtained. Glossopharyngeal n. block can be used in most patients who need atraumatic, sedated, spontaneously ventilated, "awake" TI.
Anatomy:
The glossopharyngeal n. exits from the jugular foramina at the base of the skull, in close association with other structures of the carotid sheath, vagus n., and styloid process. It descends in the neck, passes between the internal carotid and the external carotid arteries, and then divides into pharyngeal branches and motor branches to the stylopharyngeus muscle as well as branches innervating the area of the palatine tonsil and the posterior third of the tongue. These distal branches of the glossopharyngeal n. are located submucosally immediately posterior to the palatine tonsil, deep to the posterior tonsillar pillar.
a) Intraoral approach (Fig. 2):
After topical anesthesia of the tongue, the patient's mouth is opened widely, and the posterior tonsillar pillar (palatopharyngeal fold) is identified by using a No. 3 Macintosh laryngoscope blade. Then an angled 22-gauge, 9-cm needle, (this can be done by using a 22-gauge disposable spinal needle. In an aseptic manner, the stylet is removed from the disposable spinal needle and discarded. Subsequently, the distal 1 cm of the needle is bent to allow more control during submucosal insertion) and is inserted at the caudad portion of the posterior tonsillar pillar. The needle tip is inserted submucosally, and then, after careful aspiration for blood, 5 ml of lidocaine 0.5% is injected. The block is then repeated on the contralateral side.
 |
| Fig. 2: Glossopharyngeal n. Block (Intraoral approach) |
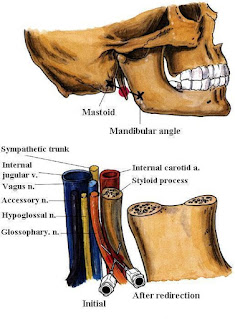
b) Peristyloid approach (Fig. 3):
The patient lies in a supine position, with the head in a neutral position. Marks are placed on the mastoid process and the angle of the mandible. A line is drawn between these two marks, and at the midpoint of that line, the needle is inserted to contact the styloid process. To facilitate styloid identification, a finger palpates the styloid process with deep pressure, and, although this can be uncomfortable for the patient, the short 22-gauge needle is then inserted until it impinges on the styloid process. This needle is then withdrawn and redirected off the styloid process posteriorly. As soon as bony contact is lost and aspiration for blood is negative, 5-7 ml of lidocaine 0.5% is injected. The block can then be repeated on the contralateral side.
 |
| Fig. 3: Glossopharyngeal n. Block (Peristyloid approach) |
3-Translaryngeal Block:
Anatomy (Fig. 4):
Translaryngeal block is most useful in providing topical anesthesia to the laryngotracheal mucosa innervated by branches of the vagus nerve. Both surfaces of the epiglottis and laryngeal structures to the level of the vocal cords receive innervation through the internal branch of the superior laryngeal nerve, a branch of the vagus. The distal airway mucosa also receives innervation through the vagus nerve but via the recurrent laryngeal nerve. Translaryngeal injection of local anesthetic helps provide topical anesthesia for both these vagal branches, since injection below the cords through the cricothyroid membrane results in solution being spread onto the tracheal structures and coughed onto the more superior laryngeal structures.
Technique (Fig. 4):
The patient should be in a supine position, with the pillow removed and the neck slightly extended. The anesthetist should be in a position to place the index and third fingers in the space between the thyroid and the cricoid cartilage (cricothyroid membrane). The cricothyroid membrane should be localized, the midline identified, and the needle, 22-gauge or smaller, inserted into the midline until air can be freely aspirated. When air can be freely aspirated, 3-4 mL of 4% lidocaine is rapidly injected. The needle should be removed immediately since it is almost inevitable that the patient will cough at this point. Conversely, a needle-over-the-catheter assembly (intravenous catheter) can be used for the block. Once air has been aspirated, the inner needle is removed, and the injection is performed through the catheter.
 |
| Fig. 4: Translaryngeal Block |
Potential Problems:
This block can result in coughing, which should be considered in patients in whom coughing is clearly undesirable. The midline should be used for needle insertion since the area is nearly devoid of major vascular structures. Conversely, the needle does not need to be misplaced far off the midline to encounter significant arterial and venous vessels.
























