Diabetic Ketoacidosis (DKA)
Physiology:
Hyperglycemia:
➧ Increased hepatic production of glucose.
➧ Diminished glucose uptake by peripheral tissues.
➧ Insulinopenia / Hyperglucagonemia.
Ketoacidemia:
➧ The ketoacid is acetoacetic acid. The byproduct is acetone. The non-keto-acid is beta-hydroxybutyric acid.
➧ Increased lipolysis and hepatic ketogenesis
➧ Reduced ketolysis by insulin-deficient peripheral tissues.
Fluid and Electrolyte Depletion:
➧ Osmotic diuresis and dehydration due to hyperglycemia.
➧ On average, water deficit is about 5L, sodium 500 mmol, potassium 400 mmol, and chloride 400 mmol.
General Considerations:
➤ Initial presentation of Type I DM (Can also occur in Type II DM).
➤ Increased insulin requirements in Type I DM (Infection, Trauma, Myocardial infarction, Surgery).
➤ Mortality is 5% in patients under 40 y. Up to 20% of the elderly.
➤ Estimates of 5-8 episodes per 1000 at-risk diabetics annually.
➤ One of the more common serious complications of insulin pump users – occurs 1 per 80 months of treatment. Typically due to unrecognized pump failure.
➤ Essentials of Diagnosis:
➧ Acidosis with pH < 7.3.
➧ Serum bicarbonate < 15 .mEq/L.
➧ The serum is positive for ketones.
➧ Elevated anion gap (variable, may occur without gap).
➧ Hyperglycemia > 250 mg/dL (no correlation between the severity of hyperglycemia and severity of ketoacidosis).
Clinical picture:
Symptoms:
➧ Early: Polyuria, Polydipsia, Fatigue, N/V.
➧ Late: Stupor – Coma.
Signs:
➧ Rapid, Deep Breathing.
➧ Fruity breath odor of acetone.
➧ Tachycardia, Hypotension, mild Hypothermia.
➧ Abdominal Pain and Tenderness.
Laboratory Findings:
➧ Glycosuria 4+, Ketonuria.
➧ Hyperglycemia, Ketonemia, Low arterial blood pH, and Low plasma bicarbonate.
➧ Elevated serum potassium (despite total body potassium depletion).
➧ Elevated serum amylase (not specific for pancreatitis in this setting, use lipase).
➧ Leukocytosis.
➧ If hyperthermic, likely due to infection since pts with DKA are hypothermic if uninfected.
Management of DKA:
Insulin Replacement:
➧ Regular Insulin IV bolus 0.1-0.2 units/kg to ‘prime’ insulin receptors.
➧ Regular Insulin infusion at 0.1 units/kg/h.
➧ Then replaced with SC regular insulin when hyperglycemia and ketoacidosis are controlled.
➧ Then oral intake + SC intermediate-acting insulin.
Fluid Replacement:
➧ The typical deficit is 4-5 L.
➧ Initially, NS 1 L/h. x 2 h., then 0.5 L/h. x 1-2 h., then 200-300 mL/h. till correction.
➧ Switch to ½ NS if serum Na > 150 mEq/L.
➧ Add D5W if the glucose falls below 250 mg/dL, to maintain serum glucose 250-300 mg/dL to prevent hypoglycemia and cerebral edema.
Sodium Bicarbonate:
➧ 50 mmol
➧ Clinical benefit has not been demonstrated.
➧ Use to correct pH < 7, target pH of 7-7.2.
Potassium:
➧ 10-30 mEq/h. replacement to be started during the second or third hour of treatment.
Phosphate:
➧ Replete hypophosphatemia of < 1 mg/dL.
➧ 15 mmol K or Na phosphate in 100 mL saline.
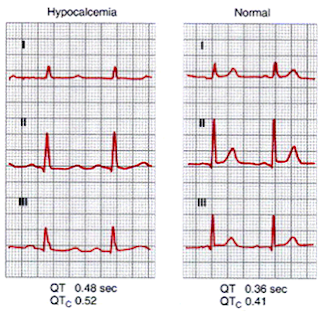
➧ Replete slowly (3-4 mmol/h.) to avoid hypocalcemic tetany.
Treatment of Associated Infection:
➧ Antibiotics: as indicated.
➧ Cholecystitis and pyelonephritis may be particularly severe in these patients.
Read more ☛ Hypoglycemic Coma