Eisenmenger’s Syndrome
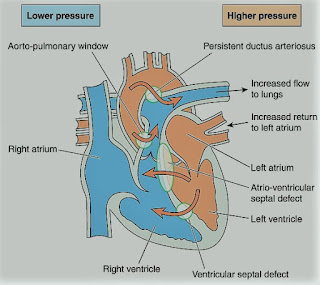
-A rare syndrome of pulmonary
hypertension associated with a reversed or bidirectional cardiac shunt,
occurring through a large communication between the left and right sides of the
heart. The defect may be interventricular, interatrial, or aortopulmonary.
-The development of Eisenmenger’s
syndrome, from the initial left to right shunt, is usually a gradual process.
Contributory factors to pulmonary hypertension are hypoxia, high pulmonary
blood flow, and high left atrial pressure.
-Irreversible structural changes
take place in the small vessels, causing pulmonary vascular obstruction and a
reduction in the size of the capillary bed. The pulmonary artery pressure is
the same as or sometimes exceeds, the systemic arterial pressure.
-The incidence of this syndrome is
decreasing because of the more vigorous approach to diagnosis and treatment of
congenital heart disease in childhood.
Preoperative Findings:
1. Presenting symptoms include dyspnea,
tiredness, episodes of cyanosis, syncope, or chest pain. Hemoptysis may occur.
2. The direction of the shunt, and
hence the presence or absence of cyanosis, depends on several factors.
These include hypoxemia, pulmonary and systemic pressure differences, and intravascular volume. It can also be affected by certain drugs.
3. Sleep studies have shown that
there is a nocturnal deterioration in arterial oxygen saturation, which seems
to be related to ventilation/perfusion distribution abnormalities occurring in
the supine position.
4. Chest X-ray shows right
ventricular hypertrophy, and ECG indicates varying degrees of right ventricular
hypertrophy and strain.
5. Complications include thrombosis
secondary to polycythemia, air embolus, bacterial endocarditis, gout, cholelithiasis,
and hypertrophic osteoarthropathy. A cerebral abscess may occur secondary to clot
embolism.
Anesthetic Problems:
1. Reductions in systemic arterial
pressure by myocardial depression or loss of sympathetic tone are potentially
dangerous. Reversal of the shunt may occur, and sudden death has been reported.
Hypovolemia and dehydration are
poorly tolerated. Syntocinon may cause a dramatic reduction in SpO2
secondary to vasodilatation.
2. Sinus tachycardia results from
exercise or emotion, and episodes of SVT are common after the age of 30. The
onset of atrial fibrillation is associated with a sudden deterioration in the
condition of the patient.
3. General anesthesia tends to be
favored since the reduction in systemic vascular resistance associated with
regional blockade increases the shunt. However, successful use of epidural anesthesia
for bilateral inguinal herniorrhaphy, and Cesarean section, have been reported.
4. Pregnancy is contraindicated
because it carries considerable risks. Recent maternal mortality rates of 40%
have been reported. A cesarean section may increase it to over 60%. Termination
of pregnancy is usually recommended in the first trimester but is still
associated with a mortality of 7%.
5. Patients are at risk from
paradoxical air or clot embolism, and infective endocarditis.
Anesthetic Management:
1. Understanding the
pathophysiology of the complex is essential, and both pregnancy and non-cardiac
surgery require a multidisciplinary approach.
2. Maintenance of an adequate
circulating blood volume is important. Myocardial depressants and peripheral
vasodilators should be used with caution. Bradycardia must be prevented. If
regional anesthesia is used, the block should be instituted with caution, and
hypovolemia avoided.
3. It is unclear whether
oxygen can cause pulmonary vasodilatation. Although the pulmonary vascular
resistance was believed to be fixed in pulmonary hypertension, a high oxygen
concentration has been shown to reduce it during cesarean section.
4. Maintenance of systemic vascular
resistance is critical. The use of a norepinephrine infusion before induction
has been described. Alpha-adrenergic vasopressors, such as methoxamine or
phenylephrine, have also been used for the treatment of hypotension on
induction of anesthesia.
5. Pulmonary ventilation should be
performed with low inflation pressures and early tracheal extubation is
advised, because of the deleterious effects of IPPV.
6. Air must be completely eliminated
from all intravenous lines and the epidural space should be located with loss
of resistance to saline, not to air.
7. Antibiotic prophylaxis against bacterial
endocarditis.
8. Low-dose heparin may reduce the
risk of emboli.
9. Patients are usually advised
against pregnancy. If anesthesia is required either for termination of
pregnancy or operative delivery, intensive cardiac care is indicated. It has
been suggested that those reaching the end of the second trimester should be
admitted to the hospital until delivery and given heparin 20000-40000 units daily and
oxygen therapy. Successful epidural anesthesia has been reported for cesarean
section.