Coarctation of Aorta
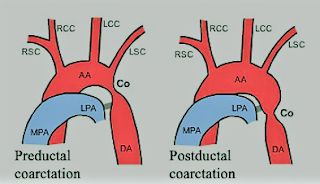
-A congenital narrowing of the aorta
that may be pre- or post-ductal.
-The preductal form is usually a
long, narrow segment, and is associated with other cardiac defects. This type
generally presents with heart failure before the age of 1 year and requires
treatment in a pediatric cardiac surgical unit.
-The postductal form, however, is
often asymptomatic, and the patient may present in later life for surgery of
some other condition, or for correction of the coarctation itself. Even after
correction of coarctation, abnormalities can continue.
-Those who have undergone repair
show persistent alterations in left ventricular function and left ventricular
mass, together with resting gradients between the arm and leg. There is a
higher incidence than normal of ischemic heart disease and sudden death.
-The optimal time for repair is
disputed. Hypertension is more common in late correction, but repair at a young
age is associated with a higher risk of recoarctation. In addition, persistent
abnormalities in aortic stiffness have been found.
-Adult repairs are associated with a
higher incidence of significant aortic valve disease (58%), compared with 37%
of those repaired in childhood.
Preoperative Findings:
1. There may be moderate
hypertension, the arm blood pressure being higher than that in the leg. If the
left subclavian arises at or below the constriction there may be an absent or
reduced left radial pulse. If both radial and femoral pulses are felt together,
the small volume and delay of the femoral pulse will be obvious.
2. Collateral circulation develops
in the internal mammary, intercostal, and subscapular arteries. The latter may
be seen if the scapula is illuminated from the side.
3. A systolic murmur is usually
heard along the left sternal edge radiating up into the neck.
4. Chest X-ray may show notching of
the undersides of the ribs, secondary to intercostal arteries dilatation. There
may be pre-and post-stenotic dilatation of the aorta.
5. Occasionally, cerebral berry
aneurysms coexist with coarctation. In such cases, the high arterial pressure
increases the risk of subarachnoid hemorrhage.
6. There is a 25–50% incidence of the bicuspid aortic valve and some aortic regurgitation.
7. Unusually, angina or left
ventricular failure may present late in untreated adult coarctation.
8. Patients may require balloon
dilatation or surgical resection.
Anesthetic Problems:
1. Before elective surgery, if undiagnosed
coarctation is found, treatment of the coarctation may be considered to be the
priority. Even if coarctation has been treated, the possibility of residual
cardiovascular abnormalities should be considered, since there is an increased
risk of premature death compared with the normal population. Causes include
aneurysms (cerebral, at the operative site, other parts of the aorta and
intercostal arteries), hypertension, myocardial infarction, and cardiac
failure. Balloon angioplasty may carry less risk.
2. Patients may present with hypertension-related
complications.
3. Any operation in the area of the
dilated collateral vessels may result in heavy bleeding, especially when the
chest is opened.
4. Hypoperfusion of the spinal cord.
This may cause paraplegia, and is more likely in those patients with few
collaterals. Induced hypotension for clipping of cerebral aneurysms may
compromise spinal cord perfusion.
5. Susceptibility to bacterial
endocarditis.
6. If there are left subclavian
abnormalities, the left arm cannot be used for blood pressure monitoring.
7. Patients may present during
pregnancy with hypertension, which may be confused with preeclampsia.
Anesthetic Management:
1. Antihypertensive therapy should
be used until the day of operation. Beta-adrenoceptor blockers may reduce the
hypertensive response to intubation.
2. Antibiotic prophylaxis against bacterial
endocarditis.
3. During clipping of an
intracranial aneurysm, monitoring of the femoral artery pressure should be
undertaken to assess spinal cord perfusion during induced hypotension. A mean
distal aortic pressure above 50 mmHg has been suggested as adequate for
spinal cord perfusion.