Tetralogy of Fallot
-Tetralogy of Fallot (TOF) is a congenital cardiac abnormality.
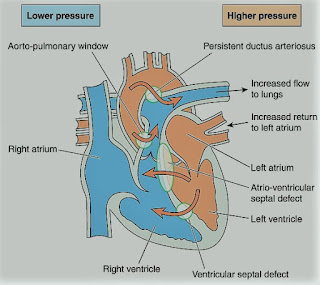
The primary defects are pulmonary infundibular stenosis and ventricular septal defect (VSD). The VSD is
sufficiently large for the pressure in both ventricles to be equal to that of
the aorta. The tetralogy is completed by two secondary features, a variable
degree of overriding of the aorta, and right ventricular hypertrophy.
-Dynamic right ventricular outflow
obstruction may occur (infundibular spasm), which is accentuated by sympathetic
stimulation. The fraction of the right to left-shunt depends primarily upon the
relative resistances between the pulmonary (or right ventricular) and systemic
outflows.
-If TOF is associated with patent foramen ovale (PFO) or atrial septal defect (ASD), it is a Pentalogy of Fallot.
-The aim of the surgery is to relieve
the right ventricular outflow obstruction and to close the VSD. The traditional
management by a two-stage repair has been replaced by definitive correction.
Recent surgical advances include conduits to connect the RV to the PA and
transatrial repair of the VSD.
The problems encountered during anesthesia
will depend upon whether or not corrective surgery has been undertaken, and the
functional result.
Preoperative Findings:
1. Dyspnea may occur on exertion and is hypoxia-related. Cyanosis and finger clubbing are variable, depending on
the degree of pulmonary stenosis and the size of the shunt. Polycythemia (erythrocytosis)
is common. There is a pulmonary stenotic murmur, but no murmur from the VSD
because of the size of the defect. Squatting is thought to reduce the fraction
of the shunt since kinking the large arteries increases systemic
vascular resistance. Squatting is commonly seen in children with uncorrected
lesions.
2. ECG shows right atrial and right
ventricular hypertrophy, right axis deviation, and right bundle branch block.
3. Echocardiography shows right atrial and right ventricular hypertrophy, VSD, PFO or ASD, pulmonary hypertension, and overriding of the aorta.
4. Chest X-ray shows right ventricular
hypertrophy and oligemic lungs. In the 2.6–6% of individuals who also have an
absent pulmonary valve, aneurysmal dilatation of the pulmonary arteries may
cause bronchial compression.
5. Initial surgery may have been
undertaken to anastomose a systemic to a pulmonary artery, to improve the
pulmonary blood flow, and reduce cyanosis. A definitive procedure is now more
commonly undertaken in infancy.
6. In patients who have undergone
shunt surgery without a definitive repair, there is chronic hypoxia and
polycythemia. These patients have a high mortality, and an increased risk of
bacterial endocarditis, thrombotic stroke, emboli, and intracerebral abscess.
7. In adults who have undergone
repair there is an increased risk of arrhythmias, conduction defects, and
sudden deaths, possibly related to mechanical events, such as ventricular
dilatation and stretch, in the proximity of the conduction system. However, new
approaches to surgery may result in a lower incidence of such problems in the
future.
Anesthetic Problems:
1. In individuals with uncorrected
lesions, the right to left shunt, and hence the cyanosis, is increased by a
reduction in systemic vascular resistance produced by systemic vasodilatation.
This may result from factors such as hypovolemia, drug effects, or pyrexia.
2. Cyanosis is also worsened by an
increase in pulmonary vascular resistance or spasm of the right ventricular
infundibulum. Right ventricular outflow obstruction is due to increased contractility which is produced by increases in
catecholamine output or the administration of drugs with positive inotropic
effects. Anxiety, pain, hypercarbia, hypoxia, and acidosis are all precipitating
factors. These cyanotic attacks or ‘tet’ spells, which can occur when awake or
under anesthesia, may initiate a cycle of increasing hypoxia that can result in
cerebral damage or death. Direct intraoperative observations of shunt direction
and flow have been made with Doppler color flow imaging using epicardial leads.
Patients with severe life-threatening hypoxemic spells, refractory to other
treatments, responded to phenylephrine (5 mcg/kg plus an infusion of 0.4–2 mcg/kg/min).
3. Dehydration in the presence of
polycythemia and high plasma viscosity may combine to increase the incidence of
cerebral thrombosis. Polycythemia may also be associated with coagulation
defects.
4. In patients with an absent
pulmonary valve, positional airway compromise occurred secondary to bronchial
compression of dilated pulmonary arteries.
5. A significant incidence of tracheal
anomalies has been found.
6. In adults who have undergone
repair, ventricular and atrial arrhythmias are common, particularly during
exercise. It has been suggested that patients scheduled for elective surgery
should have Holter monitors, or undergo exercise testing, in case antiarrhythmic
treatment is needed first.
7. Cyanosed patients with Fallot’s
rarely become pregnant. However, adults who have undergone corrective surgery are increasingly present during pregnancy with a favorable outcome.
Anesthetic Management:
1. Antibiotic prophylaxis against
bacterial endocarditis.
2. A good premedication (morphine sulphate, or midazolam) to prevent
excitement and anxiety.
3. In patients with cyanosis,
measures are aimed at reducing the right to left shunt. Specific treatments for
cyanotic attacks include:
a) Oxygen 100% to decrease PVR.
b) Pressor agents, such as
phenylephrine (5-10 mcg/kg), to increase systemic vascular resistance.
c) Fluids to correct hypovolemia.
d) Propranolol (0.1 mg/kg) or Esmolol (0.5 mg/kg) to decrease outflow
tract obstruction (decrease contractility and infundibular spasm).
e) Deepening of light anesthesia to
reduce tachycardia associated with catecholamine output.
f) Compression of the femoral artery or the abdominal
aorta against the vertebrae, sufficiently firmly to stop the femoral artery
pulsations.
4. Techniques to avoid hypoxia and
hypercarbia, and minimize vasodilatation and sudden increases in cardiac
output. Ketamine, and Morphine sulphate (0.05-0.1 mg/kg),
have been used.
5. Hydration is maintained in the
perioperative period and, if there is severe polycythemia, venesection may be
necessary.
6. Metabolic acidosis should be
prevented or treated with sodium bicarbonate (1-2 mmol/kg).
7. In pregnancy, the outcome is
satisfactory in patients whose ventricular function is good, and in whom no
residual shunt occurs. However, close observation should be undertaken by an
experienced team.
8. Venesection for erythrocytosis
that is associated with cyanotic congenital heart disease should only take place
if there are symptoms of hyperviscosity with a hematocrit >65%, and only
provided volume replacement takes place at the same time.
9. Avoid muscle relaxants with histamine release e.g. atracurium, and use cisatracurium or rocuronium.
9. Mechanical ventilation:
-Increase FiO2
-Avoid increased airway pressure (< 15 cmH2O)
-Increase respiratory rate
-Avoid PEEP