Anesthetic Considerations for Patients with Liver Disease
Preoperative:
1. Assess the Degree of hepatic impairment, Severity, and Hepatic reserve by the Child-Turcotte-Pugh
scoring system.
2. AVOID:
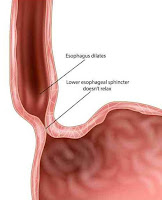
Premedication, IM injections, Contact with blood or body fluids, unnecessary
esophageal instrumentation.
Regional Anesthesia:
-Regional anesthesia might be used when possible in patients with
advanced liver disease.
-Coagulopathy (PT & INR) should be considered a
contraindication to some types of regional anesthesia.
-AVOID Epidural a. (Large amounts of amide LAs).
IV Anesthetics:
-Propofol, Ketamine (in hypotensive patients).
Opioids:
-Opioids can also be used successfully in patients with the hepatic
disease despite certain pharmacological consequences (decreased clearance and
prolonged half-life).
-Fentanyl is considered the opioid of choice because it does not
decrease hepatic oxygen and blood supply nor does it prevent increases in
hepatic oxygen requirements when used in relatively moderate doses.
-AVOID Morphine (Active metabolite, Prolonged action).
Changed Pharmacokinetics:
-The half-life of lidocaine in patients with liver disease may be
increased by more than 300%, for benzodiazepines by more than 100%, etc.
-For drugs binding to albumin, the volume of distribution is decreased
and therefore the drug dosage should be decreased (e.g. sodium pentothal).
Muscle Relaxants:
-Suxamethonium →
Prolonged action, Atracurium, Cisatracurium (of choice).
-AVOID Pancuronium, Vecuronium (Hepatic metabolism).
-The volume of distribution of many drugs can be substantially
increased (for different reasons, including an increase in gamma globulin and edema),
dictating a necessity to increase the first effective dose of the drug.
-However, owing to a decrease in hepatic blood flow and hepatic
metabolic and excretory functions, as well as impaired renal function, the clearance
of such a drug is decreased, therefore the effect can be prolonged (e.g. pancuronium).
-Atracurium has a theoretical advantage because its metabolism is not
dependent on liver function. Therefore, the clearance
and elimination half-life of atracurium in patients with impaired hepatic
and/or renal function is not different from those with normal
hepato-renal function. However, the volumes of distribution are larger, and,
accordingly, the distribution half-lives are shorter in patients with severe
hepato-renal dysfunction compared with normal individuals.
-Titration of any relaxant according to the transcutaneous nerve
stimulation monitoring is beneficial because the degree of hepatic dysfunction
affects the degree of pharmacokinetic disorders.
Inhalational Anesthetics:
-Halothane
should be avoided because it leads to the most prominent decrease in hepatic
blood flow and oxygen supply and postoperative hepatic dysfunction. In
addition, immunologically mediated severe postoperative halothane hepatitis may
follow halothane anesthesia.
-Isoflurane is a better choice if an inhalational technique is selected.
-More recently
introduced volatile anesthetics, sevoflurane, and desflurane, each of them, can
be used safely in patients with liver disease, as they preserve hepatic blood
flow.
-Nitrous oxide
has been used in patients with advanced hepatic disease for many years, and so
far has not been incriminated in increased anesthesia-related hepatic
postoperative complications. However, a well-known sympathomimetic effect of
nitrous oxide and some possibilities of jeopardizing oxygenation render the
routine use of nitrous oxide in patients with advanced liver disease undesirable.
It is important to remember that long surgical operations under anesthesia with
nitrous oxide might result in the accumulation of nitrous oxide in the
intestinal lumen with subsequent intestinal distension.
Others:
-Renal function must be maintained by administering proper fluid
load (volume and content); (avoid Na+ overload, use glucose-containing
solutions for hypoglycemia, albumin 5% is the preferred colloid), and diuretics
if needed.
-The parameters of controlled ventilation should be carefully
selected to avoid an unnecessary increase in intrathoracic pressure
which may impede venous return thereby decreasing cardiac output.
-Monitoring the coagulation state during surgery can be important. The treatment should be based on the results of hematologic monitoring and may include administration of platelets, fresh frozen plasma, cryoprecipitate, and sometimes tranexamic acid.